The following resources are available to support with Asthma management.
Accessing CDRC resources on SystmOne
To access the below resources you will need to be a member of the DCS group on SystmOne. To do this, please follow the instructions on the CDRC SystmOne Access webpage.
Asthma Quality Improvement Reports
A series of reports are available to help improve asthma care and identify high risk patients.
These reports are in the folder CDRC Quality > Respiratory
They are also described in a Reports tab on the Asthma CDRC template.
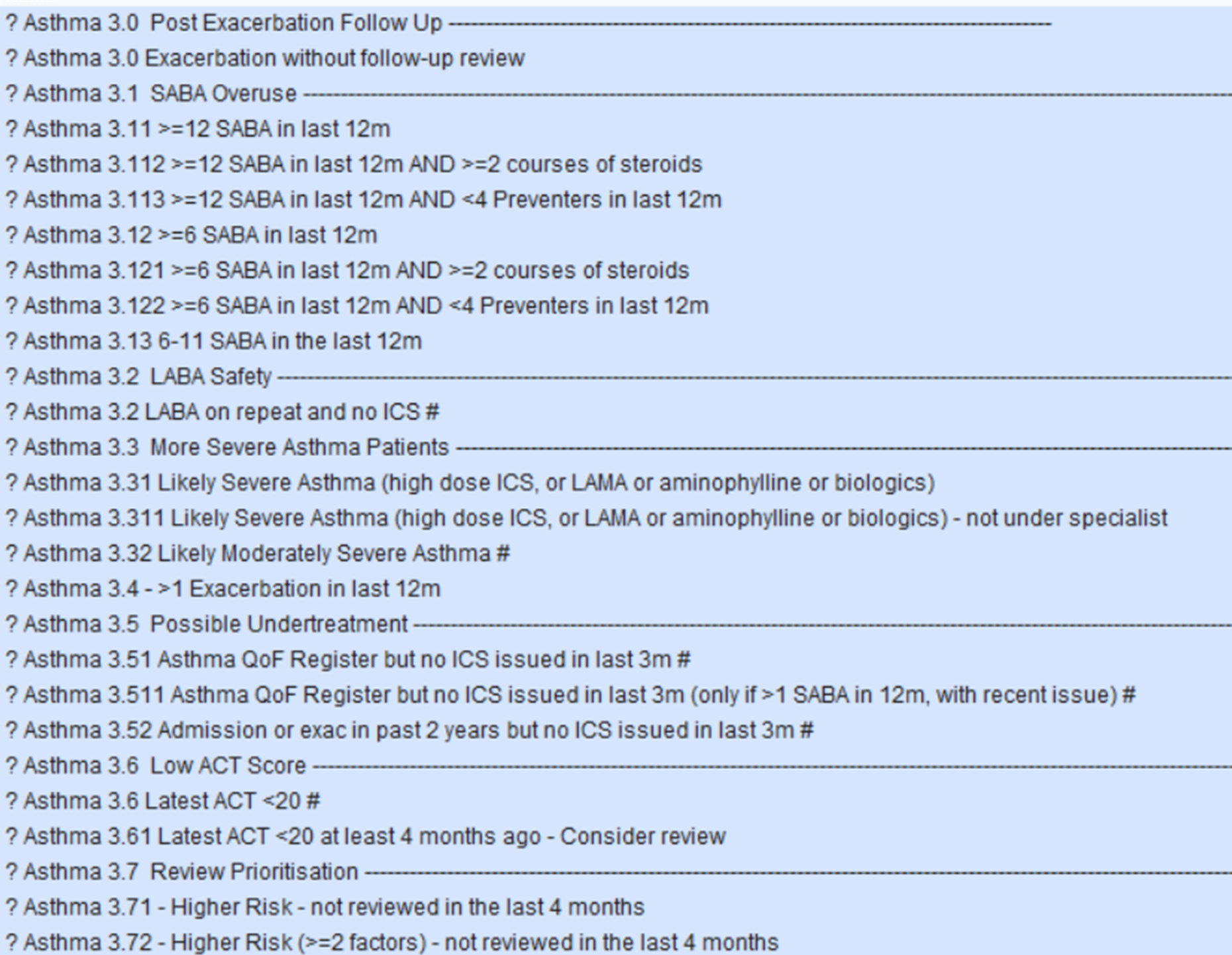
| Report Name | Returns |
| ? Asthma 3.0 Post Exacerbation Follow Up | —————————————————————————————– |
| ? Asthma 3.0 Exacerbation without follow-up review | Patients who have had an exacerbation in the last year without a subsequent follow-up review |
| ? Asthma 3.1 SABA Overuse | —————————————————————————————– |
| ? Asthma 3.11 >=12 SABA in last 12m | Asthma patients (excluding COPD) receiving treatment that have been issued 12 SABAs in the last 12 months. |
| ? Asthma 3.112 >=12 SABA in last 12m AND >=2 courses of steroids | Asthma patients (excluding COPD) receiving treatment that have been issued 12 SABAs AND equal to, or more than, 2 courses of steroids in the last 12 months. |
| ? Asthma 3.113 >=12 SABA in last 12m AND <4 Preventers in last 12m | Asthma patients (excluding COPD) receiving treatment that have been issued 12 SABAs AND less than 4 ICS in the last 12 months. |
| ? Asthma 3.12 >=6 SABA in last 12m | Asthma patients (excluding COPD) receiving treatment that have been issued 6 SABAs in the last 12 months. |
| ? Asthma 3.121 >=6 SABA in last 12m AND >=2 courses of steroids | Asthma patients (excluding COPD) receiving treatment that have been issued 6 SABAs AND equal to, or more than, 2 courses of steroids in the last 12 months. |
| ? Asthma 3.122 >=6 SABA in last 12m AND <4 Preventers in last 12m | Asthma patients (excluding COPD) receiving treatment that have been issued 6 SABAs AND less than 4 ICS in the last 12 months. |
| ? Asthma 3.2 LABA Safety | —————————————————————————————– |
| ? Asthma 3.2 LABA on repeat and no ICS | Asthma patients with LABAs on repeat but no ICS. |
| ? Asthma 3.3 More Severe Asthma Patients | —————————————————————————————- |
| ? Asthma 3.31 Likely Severe Asthma (high dose ICS, or LAMA or aminophylline or biologics) | Asthma patients that are likely to have severe asthma as they one of the following medications on repeat; a high dose ICS, theophylline/ aminophylline, LAMA, respiratory immunotherapy. |
| ? Asthma 3.311 Likely Severe Asthma (high dose ICS, or LAMA or aminophylline or biologics) – not under specialist | Asthma patients with one of the following medications on repeat; a high dose ICS, theophylline/ aminophylline, LAMA, respiratory immunotherapy – ARE NOT under the care of a respiratory specialist or community team. |
| ? Asthma 3.32 Likely Moderately Severe Asthma | Asthma patients with possible high dose ICS on repeat. |
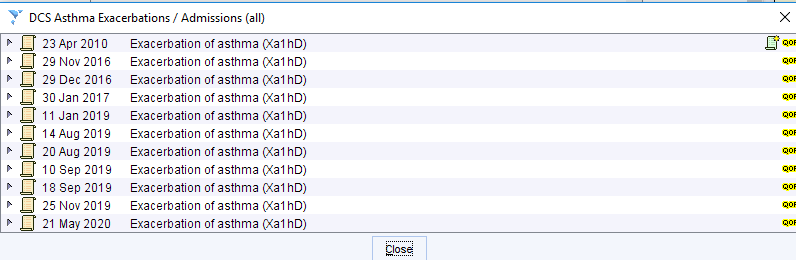
| ? Asthma 3.4 >1 Exacerbation in last 12m | Patients which have had at least 1 exacerbation in the last 12 months. |
| ? Asthma 3.5 Possible Undertreatment | —————————————————————————————– |
| ? Asthma 3.51 Asthma QoF Register but no ICS issued in last 3m | Patients on the Asthma QoF register that have not had an ICS issued in the last 3 months. |
| ? Asthma 3.511 Asthma QoF Register but no ICS issued in last 3m (only if >1 SABA in 12m, with recent issue) | Patients on the Asthma QoF register that have not had an ICS issued in the last 3 months. Have had at least one SABA issued in last 12 months AND a SABA issued in the last 4 months. |
| ? Asthma 3.52 Admission or exac in past 2 years but no ICS issued in last 3m | |
| ? Asthma 3.6 Low ACT Score | —————————————————————————————– |
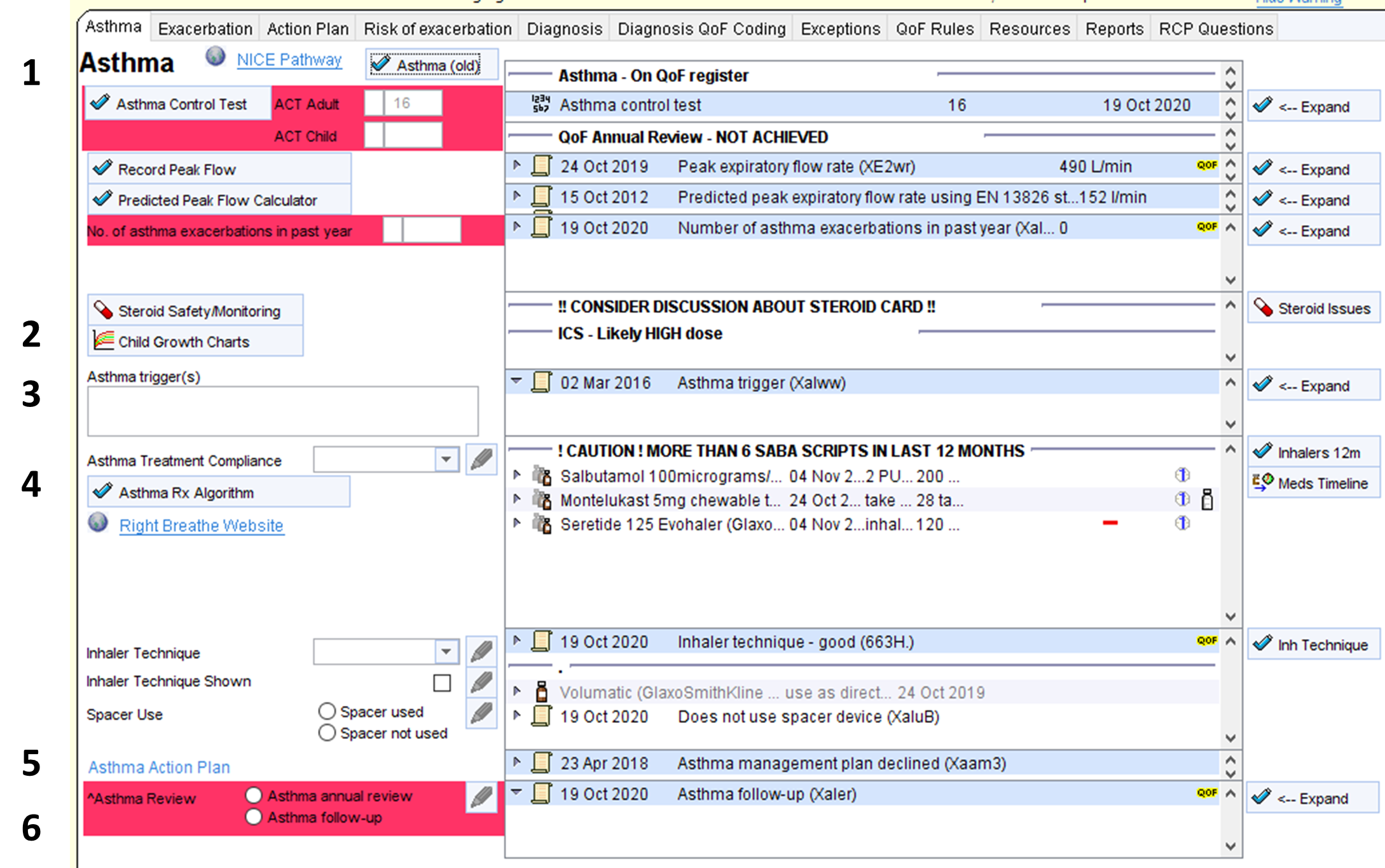
| ? Asthma 3.6 Latest ACT Score <20 | Patients whose asthma does not appear to be controlled. |
| ? Asthma 3.61 Latest ACT <20 at least 4 months ago – Consider review | Patients whose asthma did not appear to be controlled at least three months ago and who haven’t subsequently reported an improvement. These patients could be followed up or asked to repeat the ACT test in person or online. |
| ? Asthma 3.7 Review Prioritisation | —————————————————————————————– |
| ? Asthma 3.71 Higher Risk – not reviewed in last 4 months | Asthma patients with indicators of poor control who haven’t been reviewed in the last 4 months. |
| ? Asthma 3.72 Higher Risk – (>=2 factors) – not reviewed in the last 4 months | As Above – increased level of risk. |
| ? Asthma 3.73 Higher Risk – (>=3 factors) – not reviewed in the last 4 months | As Above -increased level of risk. |
| ? Asthma 3.74 Higher Risk – (>=4 factors) – not reviewed in the last 4 months | As Above -increased level of risk. |
Additional reports to help improve care of all Respiratory Diseases
The following reports below are located in the folder CDRC Quality > Respiratory
These reports could be added to a batch reporting process so the relevant person or team in the practice is notified of the results at regular intervals for an ongoing quality improvement process – Automated Reporting
Asthma CDRC Template
How to Access
In the lower left hand corner use the search bar, type in ‘Asthma CDRC’ and select the following template:
Alternatively, press F12 and search for ‘Asthma CDRC’, this will return the aforementioned template.
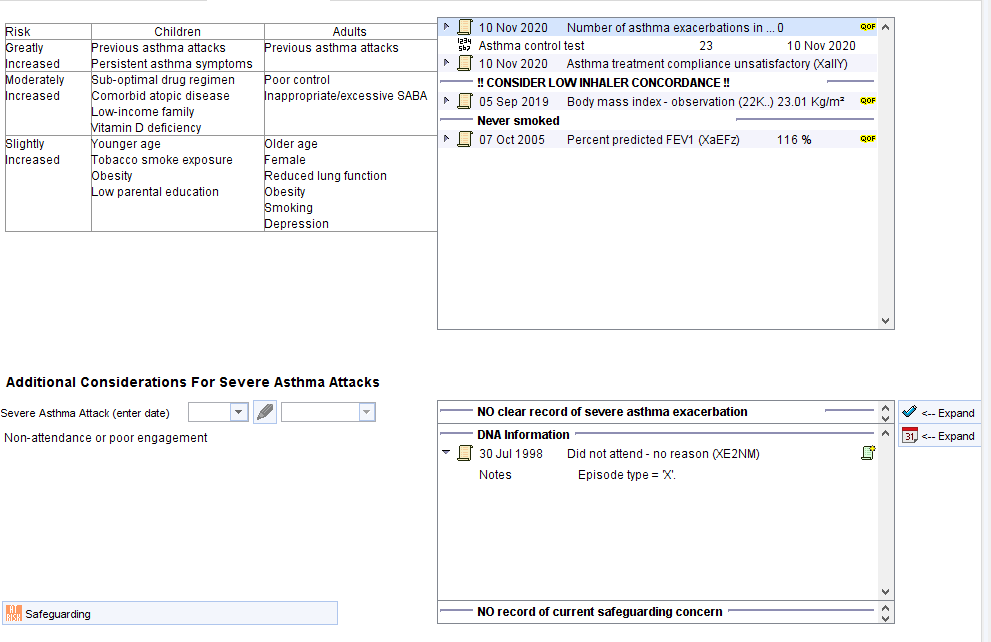
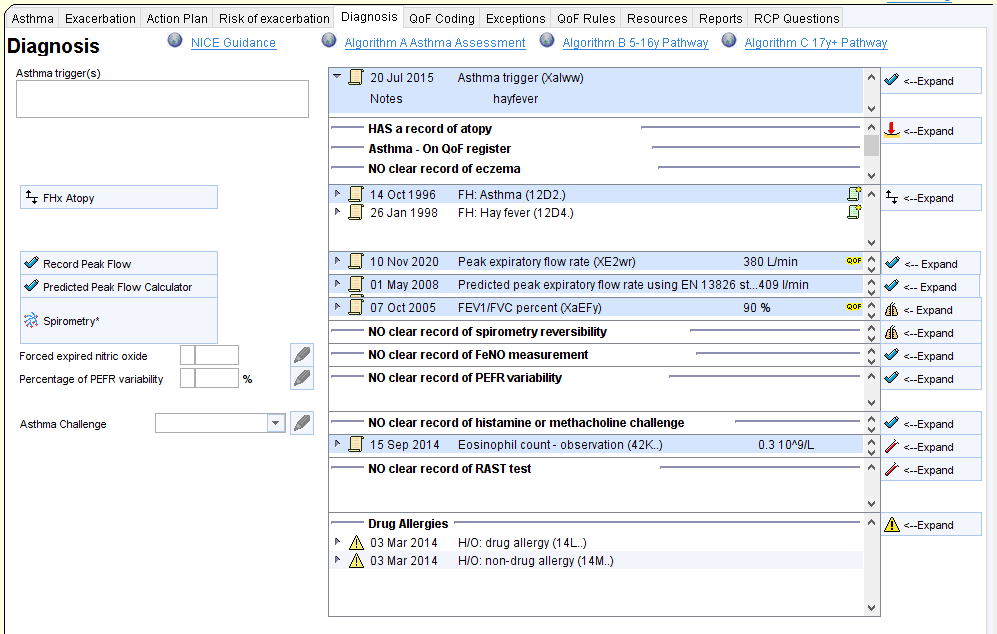
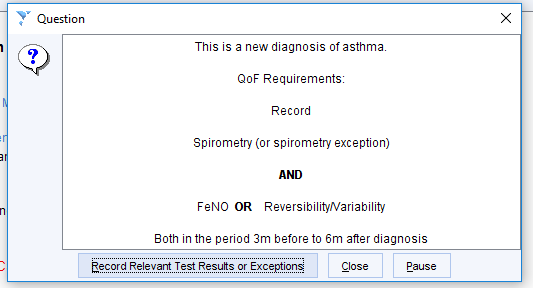
The Asthma CDRC Template can be used during consultations to provide an overview of current asthma issues, recording of key information, creating/ updating the patient’s personal action plan and more. Expand each node below to view information on each page of the Asthma CDRC template.
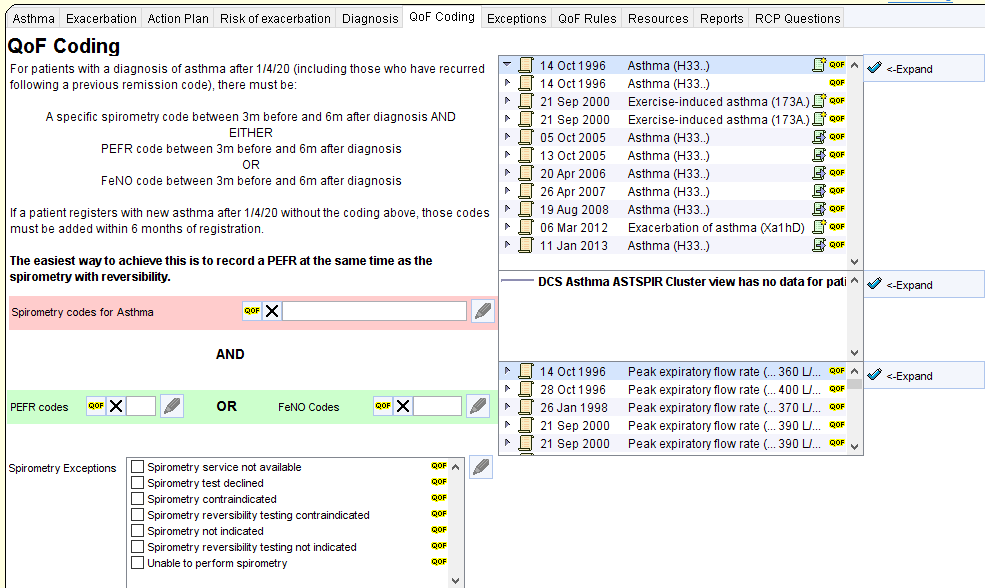
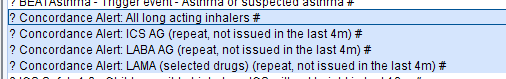
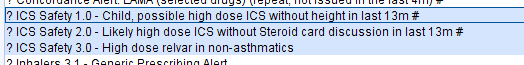
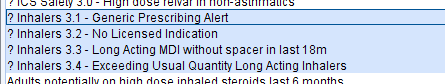
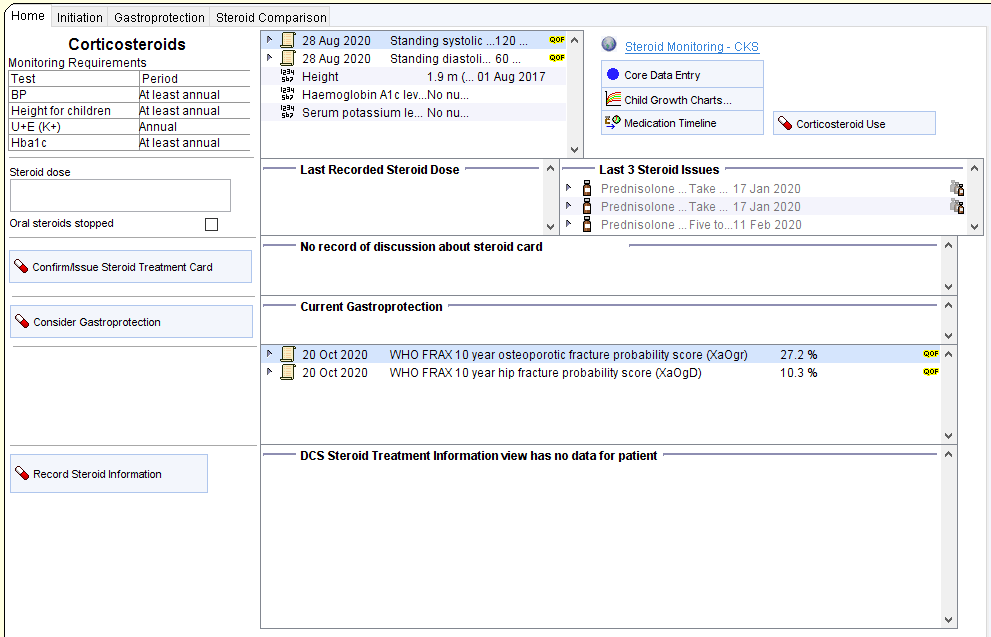
Opt-in Resources
The coding requirements for asthma are increasingly complex (and at times nonsensical). The following resources will help keep on top of this. As they are a little intrusive, these protocols need to be enabled at individual practices or CCGs. Contact contact-cdrc@ahsn-nenc.org.uk to enable them
Improve coding of asthma exacerbations
This protocol will trigger for patients with asthma who are prescribed oral steroids if they have not had a code for exacerbation of asthma recorded during the same consultation.
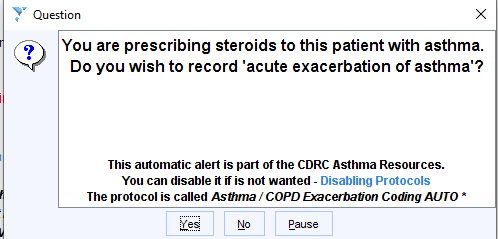
If the patient has COPD and asthma you will be offered the option of coding exacerbation of asthma or COPD or both.
Whenever exacerbation of asthma is coded a prompt will be displayed to advice the user to arrange a follow up within a few days.
Warning if a new diagnosis of asthma is recorded and the QoF business rules for recording spirometry, peak flow and FeNO have not been satisfied.
The following report will identify patients with a relevant new diagnosis without appropriate diagnostic tests. You may wish to add this to an Automated Reporting process.
CDRC Quality > Respiratory > ? Asthma QoF 1.0 – Diagnostic Tests Missing

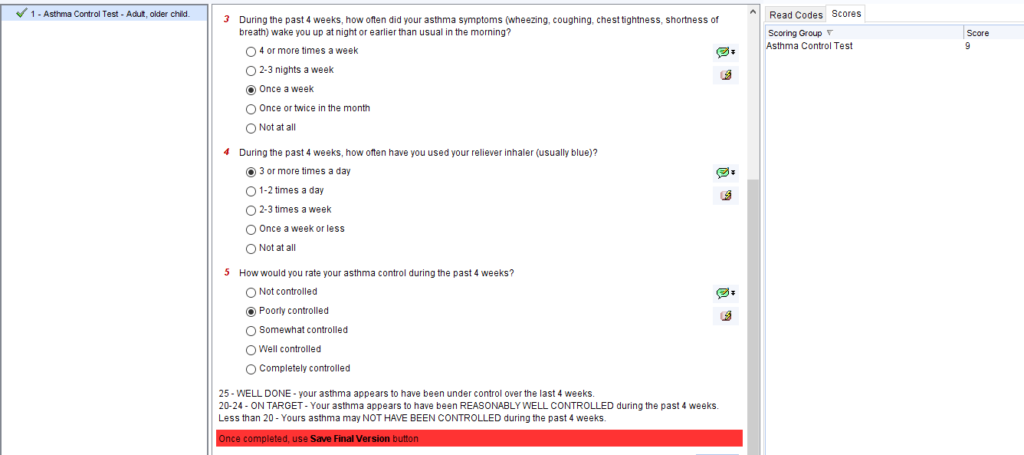
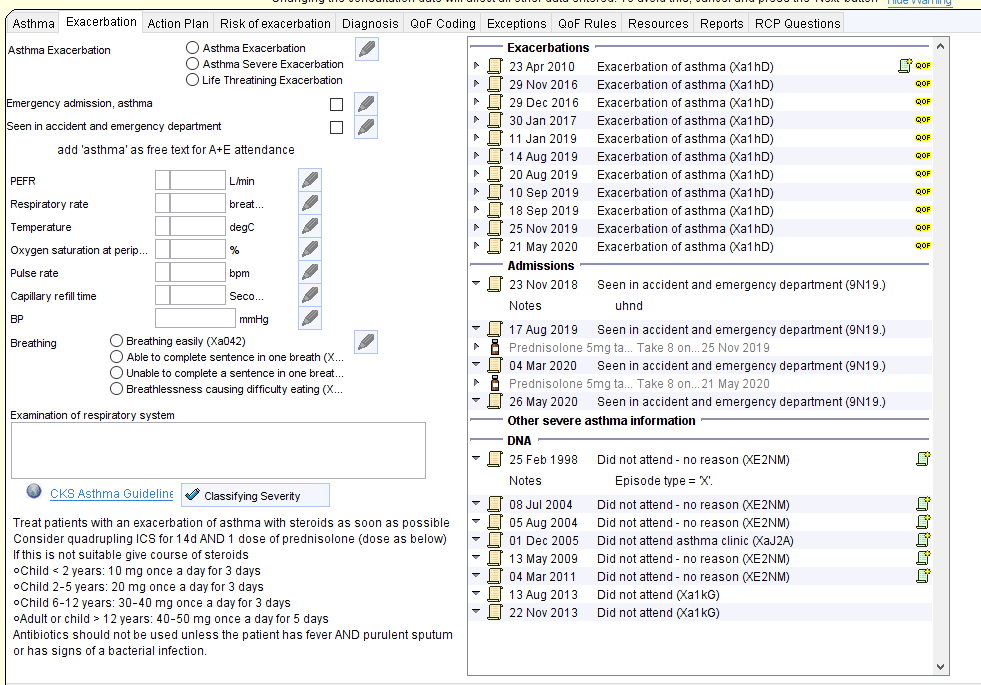
![Asthma Action Plan
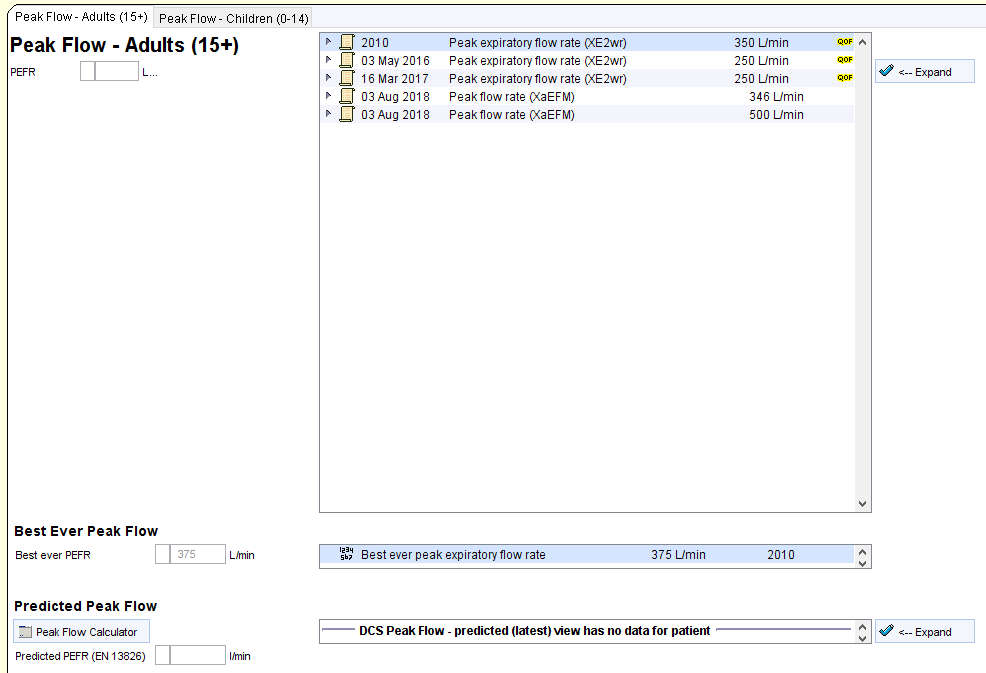
Record Peak Flow
Record Sest Ever Peak Flow
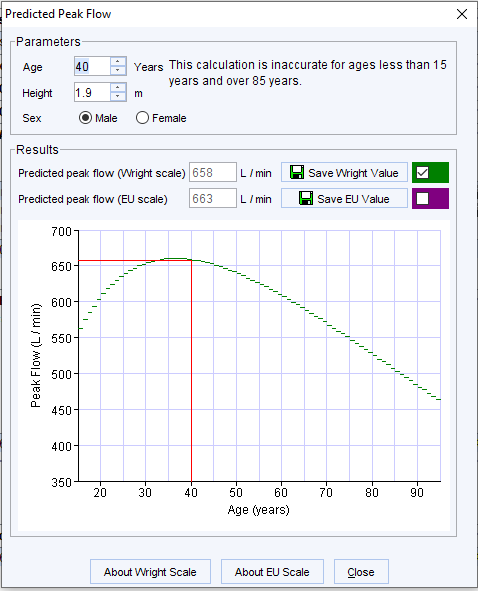
Predicted Peak Flow Calculator
PEFR 80/50/30% sand calculator
Complete Adut Action Plan
Complete Child Action Plan
Complete Seat Action Plan
Create Action Plan
26 Jun 2021 Peak expiratory flow rate
Best ever peak expiratory flow rate
400 LJmin
450 LJmin
12 Jun 2020
26 Jun 2021
Predicted peak expiratory flow rate using EN 13826 limin
Expected peak flow rate x 80%
Expected peak flow rate x 50%
Expected peak flow rate x 30%
Asthma UK Child Asthma Action Plan
320 limin
200 limin
120 limin
12 Jun 2020
12 dun 2020
12 Jun 2020
12 Jun 2020 06 28
Entered by
Finished by
FORBES, Gareth (Dr) (General Medical Practitioner)
FORBES, Gareth (Dr) (General Medical Practitioner) [12 Jun 2020 06:28]
Expand
Expand
All Plans
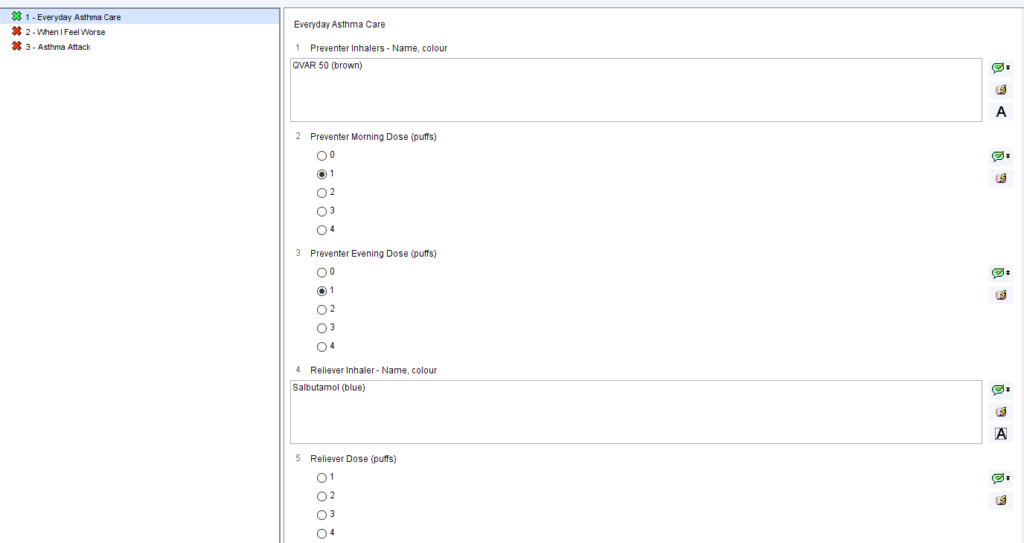
Everyday Asthma Care
Preventer- Name
Preventer- Colour
Preventer Morning Dose (puffs)
Preventer Evening Dose (puffs)
Other daily medicines
Reliever Inhaler- Name
Reliever Colour
Reliever Dose (puffs)
When I Feel Worse
Reliever Inhaler dose (puffs)
Other things to do
Pulmicorl 100
White
montelukast
Salbutamol
Blue
panic
Action Plan
C) Agreed
o
Reviewed
26 Jun 2021
26 dun 2021
9
26 Jun 2021
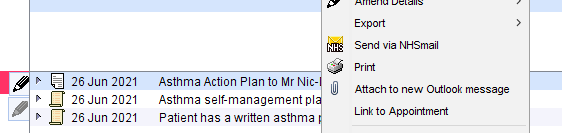
Asthma Action Plan to Mr Nic-Donotuse Mestpatientkamb
Asthma self-management plan agreed
Patient has a written asthma personal action plan
Action Plan Declined](https://cdrc.nhs.uk/wp-content/uploads/2022/11/image-66.png)