Harm caused by Opioid medication is a major cause for concern. NICE guidance recommends that Opioids are unlikely to be suitable for controlling primary chronic pain. A series of resources are available to help support harm reduction.
Population Reporting Searches
Accessing the Opioid Population Reporting Searches
To access the CDRC Opioid Population Reporting Searches / Reports on EMIS, you will need to download and import the following .zip file:
If you have not performed this process before, please refer to the Download/ Import guide below, which provides you with step-by-step instructions on how to Download and Import .zip files into EMIS:
You can check whether you have the most up-to-date version by reviewing the date on the .zip file. Any updates to the Population Reporting searches will be communicated to CDRC Precision users via the mailing list for the CDRC. To ensure you stay up to date with the latest information, please sign up to the mailing list at http://eepurl.com/9131L
Guidance on the Opioid Population Reporting Searches
The following searches are included in the above CDRC Quality Pain zip.file.
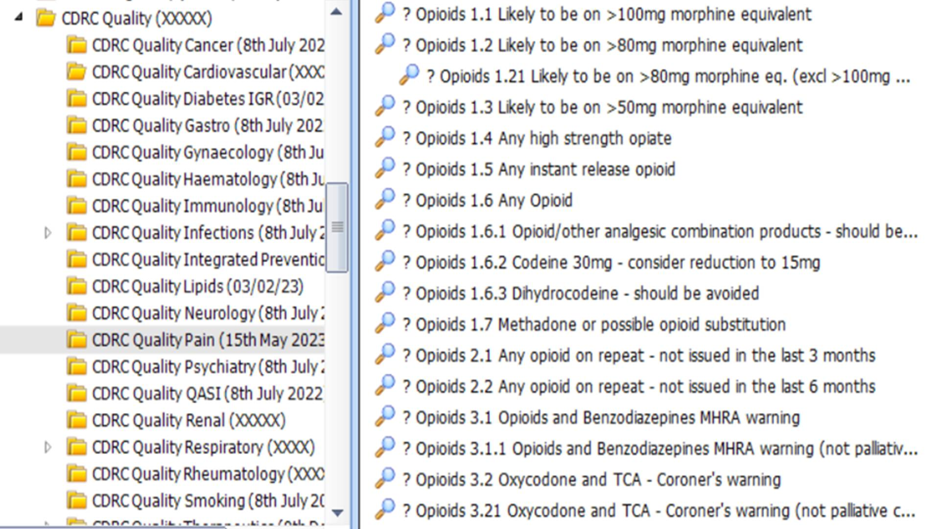
Searches ? Opioids 1.1 – 1.6 exclude patients on the palliative care register or taking methadone.
Searches ? Opioids 1.1 – 1.7 detect medication on repeat or being issued repeatedly over the past 3 months.
Tackling opioid use can feel like an overwhelming issue. The searches are designed to help divide this work into manageable chunks, starting with the highest risk patients.
| Search | Patients | Action |
| ? Opioids 1.1 Likely to be on >100mg morphine equivalent | Likely to be having medication with a morphine equivalent (Meq) dose of >100mg / day | Review patients. Patients requiring >100mg are unlikely to have an opioid responsive pain. Some guidelines recommended reduction and cessation of opioids |
| ? Opioids 1.2 Likely to be on >80mg morphine equivalent | Patients that are likely to be medication with a morphine equivalent dose of >=80mg | Review patients and consider dose reduction. |
| ? Opioids 1.21 Likely to be on >80mg morphine equivalent (excl >100mg morphine equivalent) | Patients that are likely to be medication with a morphine equivalent dose of >=80mg, excluding patients with a morphine equivalent dose of >=100mg | |
| ? Opioids 1.3 Likely to be on >50mg morphine equivalent | Likely to be having medication with a morphine equivalent (MEq) dose of >50mg / day | Review patients and consider dose reduction. |
| ? Opioids 1.4 Any high strength opiate | Patients receiving high strength opioids such as morphine, buprenorphine and fentanyl | Review patients and consider dose reduction. |
| ? Opioids 1.5 Any instant release opiate | Patients receiving instant release opioids such as oramorph or oxynorm | Guidelines suggest that instant release opioids are unlikely to be suitable for chronic pain. Review patient and consider reduction or cessation |
| ? Opioids 1.6 Any Opioid | Patients receiving any opioid | Review patients and consider dose reduction. |
| ? Opioids 1.6.1 Opioid / other analgesic combination products – should be avoided | Patients receiving combination products such as co-cocodamol or codydramol. | These products are considered to be less suitable. Review patient and consider reduction, cessation or switching to separate medications. |
| ? Opioid 1.6.2 Codeine 30mg – consider reduction to 15mg | Patients receiving codeine 30mg tablets | Patients could be offered 15mg tablets instead to allow them to take smaller doses. |
| ? Opioid 1.6.3 Dihydrocodeine – should be avoided | Patients receiving dihydrocodeine | Some areas have indicated that this drug is no longer suitable for prescribing. Review patients and consider reduction/cessation |
| ? Opioid 1.7 Methadone or possible opioid substitution | Patients likely to be receiving opioid substitution | For reference. Consider review. |
| ? Opioid 2.1 Any opioid on repeat – not issued in the last 6 months | Patients with opioid on repeat which have not been issued in the last 6 months | Consider removing from repeat prescription |
| ? Opioid 2.2 Any opioid on repeat – not issued in the last 3 months | Patients with opioid on repeat which have not been issued in the last 3 months | Consider removing from repeat prescription |
| ? Opioid 3.1 Opioids and Benzodiazepines MHRA warning ? Opioid 3.11 Opioids and Benzodiazepines MHRA warning (not palliative care) | Patients receiving opioids and benzodiazepines MHRA warning (additional search to exclude palliative care patients) | This high risk combination has a high risk of respiratory depression and review/reduction/cessation should be considered |
| ? Opioid 3.2 Oxycodone and TCA – Coroner’s warning ? Opioid 3.21 Oxycodone and TCA – Coroner’s warning (not palliative care) | Patients receiving oxycodone and tricyclic antidepressants coroner’s warning (additional search to exclude palliative care patients) | This high risk combination has a high risk of respiratory depression and review/reduction/cessation should be considered |
NIPP Project Study Guidance
The Searches required for this study are included in the above CDRC Quality Pain zip.file (Expand the Accessing the Opioid Population Reporting Searches node).
CDRC has created several searches to identify and prioritise patients currently taking opioid medication to potentially reduce their opioid dosage or to substitute their opioid medication for a safer alternative. Not all of these searches are applicable to the NHS Insights Prioritisation Programme (NIPP) opioid study.
For the NIPP Project, a member of staff at your EMIS practice will run and report on the following searches:
- ? Opioids 1.1 Likely to be on >100mg morphine equivalent
- ? Opioids 1.21 Likely to be on >80mg morphine equivalent (not >100mg morphine equivalent)
- ? Opioids 1.6 Any Opioid
These searches are found in the CDRC Quality > Pain folder and are highlighted below:
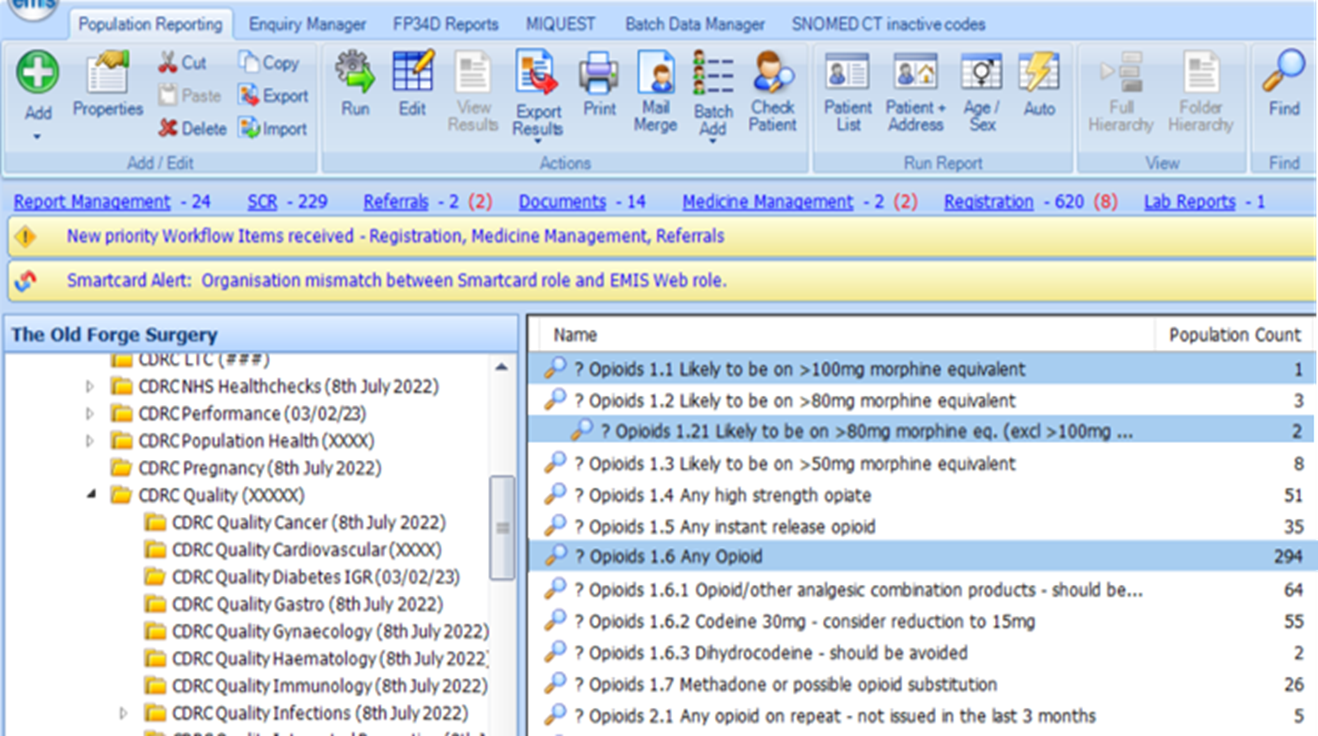
NIPP Study Criteria:
Patients targeted will include adults (aged 18 or over) registered with a mobile phone number at practices and those regularly taking opioids for more than 90 days and at dose equivalent to ≥ 90 mg equivalent of morphine a day (this varies for each opioid medication) using electronic records. Patients will be excluded if they are coded cancer or palliative care. Eligible patients will be screened and identified by primary care staff in the participating practices.
Please note:
- The highlighted searches above exclude patients on palliative care, or taking Methadone/Subutex.
- These searches include opioids on repeat prescription or >=2 scripts in the last 3 months as a proxy for usage over 90d.
- The opioid drug combination required to meet the >90mg morphine equivalence is very rare, thus CDRC has created searches ? Opioids 1.1 and ? Opioids 1.2/1.21 to reflect the inclusion criteria as closely as possible.
