A suite of Reports for SystmOne, created by the CDRC can be used identify patients in your practice who might benefit from lipid lowering or optimisation of treatment.
These reports have been categorised into 3 primary areas:
- Quality Improvement – Reports to identify patients who might benefit from lipid lowering or treatment optimisation.
- Performance – Reports to show current performance with respect to lipid management.
- Statin Safety – Reports to identify patients with significant statin safety issues.
Before starting your Lipid Management, CDRC recommends that you first run the reports in the ‘Casefinding Reports’ node to identify patients with potentially un-coded conditions that will affect decisions about lipid modification.
Casefinding Reports
We recommended that you first run the reports in each of the nodes below to identify patients with potentially un-coded conditions that will affect decisions about lipid modification.
Quality Improvement Reports
CDRC’s Quality Improvement Reports will help to identify patients who may benefit from lipid lowering or treatment optimisation, they are located in the folder CDRC Quality > Lipids.
These reports have been categorised to allow for manageable numbers of patients depending on the resource you have available.
Lipid Screening – Screening for people at risk of CVD
| Report Name | Report Returns | Notes |
| ? Lipids 1.0 Screening – Target for CVD Risk Assessment (as estimated risk is >10%) | Patients whose estimated CVD risk is >10%. Excludes: On lipid lowering therapy Recorded reason why lipid lowering therapy not being taken Established CVD or FH | Consider offering these patients a CVD risk assessment |
| ? Lipids 1.01 Screening – Target for CVD Risk Assessment – eligible for NHS HC | Patients in 1.0 who are currently eligible for and NHS Health Check | Consider offering NHS Health Check |
| ? Lipids 1.02 Screening – Target for CVD Risk Assessment – has LTC | Patients in 1.0 who also have a long term condition | Consider offering CVD risk assessment at next LTC review |
| ? Lipids 1.03 Screening – Target for CVD Risk Assessment – not eligible for NHS HC, no LTC | Patients in 1.0 who do not have a long term condition and who are not currently eligible for an NHS Health Check | Consider specific invitation for CVD risk assessment |
| ? Lipids 1.04 Screening – Target for CVD Risk Assessment – estimated risk >20% | Patients in 1.0 who have an estimated CVD risk >=20% | Consider prioritising these patients for CVD risk assessment |
Lipid Screening – Screening for Familial Hypercholesterolaemia
| Report Name | Report Returns | Action |
| ? Lipids 2.0 Case Finding – Consider screening for familial hypercholesterolamia | Patients who have a significant chance of familial hypercholesterolaemia | Screen for FH – see below |
| ? Lipids 2.01 Case Finding – Consider screening for familial hypercholesterolamia (also eligible for IFF FH referral) | Patients in 2.0 who are also appear in the IIF CVD04 ‘consider for FH assessment’ denominator | Screen for FH – see below |
| ? Lipids 2.02 Case Finding – Consider screening for familial hypercholesterolamia – highest risk patients | Patients in 2.0 who are at highest risk of FH – for areas with limited resources – concentrate on these patients | Screen for FH – see below |
| ? Lipids 2.1 Case Finding – Eligible for IFF FH referral but FH less likely | Patients who appear in the IIF CVD04 ‘consider for FH assessment’ denominator, who are less likely to have FH | Screen for FH – see below, but likely to have a secondary cause of hyperlipidaemia |
| ? Lipids 2.2 Case Finding – Code for FH but not genetic code – consider need for genetic testing | Patients with a code suggesting FH e.g. Possible FH who don’t have a definitive FH code | Review record and consider: Adding definitive code if appropriate Referral for genetic testing Removal of code if incorrect – e.g. secondary hyperlipidaemia |
Click here for further resources to assist with FH Screening.
Lipid Management – Consider Starting / Restarting Lipid Lowering
| Report Name | Report Returns | Notes |
| ? Lipids 3.0 Management – Consider Lipid Lowering | Patients who appear eligible for lipid lowering for primary or secondary prevention who don’t have a recorded reason why not. | Review patient: consider offering statin or other treatment recording ‘declined, not indicated’ etc. Record previous ADRs to lipid lowering treatment. |
This report has sub-reports which risk stratify patients so those at highest risk can be prioritised (3.01-3.06)
| Report Name | Report Returns | Notes |
| ? Lipids 3.2 Management – Possible poor lipid lowering therapy concordance | Patients with repeat lipid lowering therapy who have not been issued a prescription in the last 3 months. | Review patient – discuss concordance or remove medication from repeat if no longer necessary. |
Lipid Management – Lipid Lowering Optimisation
| Report Name | Report Returns | Notes |
| ? Lipids 4.1 Management – On lipid lowering – without a lipid target | Patients with repeat lipid lowering therapy who do not have a lipid target. | Review patient – consider adding target. The Lipid Details Template will facilitate this. |
| ? Lipids 4.2 Management – On lipid lowering – has lipid target but not achieved | Patients with a lipid target which has not been achieved. | Consider intensification of lipid treatment or relaxation of target (e.g. for frail patients). |
| ? Lipids 4.3 Management – On low/mod lipid lowering – consider intensification | Patients on moderate or low potency lipid lowering without a documented reason. There is a subset report limited to people with manifest ASCVD only. | Review patient. Consider: Intensification coding of previous ADRs to lipid lowering recording patient has reached maximally tolerated lipid lowering. Loosen target cholesterol. |
| ? Lipids 4.31 Management – On low/mod lipid lowering – consider intensification (excl. target is achieved) | As for 4.3 but excludes patients who have reached their target cholesterol There is a subset report limited to people with manifest ASCVD only. | As above. |
| ? Lipids 4.4 Management – Consider intensification to very high intensity lipid lowering | Patients eligible for secondary prevention who are not on very high intensity lipid lowering. | Review patient. Consider Intensification coding of previous ADRs to lipid lowering recording patient has reached maximally tolerated lipid lowering. Loosen target cholesterol. |
| ? Lipids 4.41 Management – Consider intensification to very high intensity lipid lowering (excl. target is achieved) | As for 4.4 but excluding patients who have reached their target cholesterol. | As above. |
| ? Lipids 4.5 Management – Consider intensification for patients with ASCVD and non-HDLC >=2.5 | Patients with established atherosclerotic ASCVD with nonHDL C unless they have achieved a stated target. | Review patient. Consider Intensification coding of previous ADRs to lipid lowering recording patient has reached maximally tolerated lipid lowering. Loosen target cholesterol. |
Lipid Management – May Need Specialist Lipid Management
| Report Name | Report Returns | Notes |
| ? Lipids 5.1 Management – Consider lipid lowering – May need more detailed input | Patients who appear to need lipid lowering but have had ADR to at least one statin AND ezetimibe | |
| ? Lipids 5.2 Management – Criteria for PCSK9i but poor concordance with current treatment | Fulfil referral criteria for PCSK9i therapy but may not be taking current lipid lowering therapy | Review concordance |
| ? Lipids 5.3 Management – Criteria for PCSK9i – Consider primary care intensification | Fulfil referral criteria for PCSK9i therapy but there may be scope for intensification of lipid lowering therapy in primary care | Review record |
| ? Lipids 5.4 Management – Criteria for PCSK9i – Consider referral ** | Likely to be eligible for PCSK9i referral | Consider referral |
| ? Lipids 5.5 Management – Criteria for Inclisiran – But poor concordance with current treatment | Fulfil referral criteria for inclisiran therapy but may not be taking current lipid lowering therapy | Review concordance |
| ? Lipids 5.6 Management – Criteria for Inclisiran – Consider primary care intensification | Fulfil referral criteria for inclisiran therapy but there may be scope for intensification of lipid lowering therapy in primary care | Review record |
| ? Lipids 5.7 Management – Criteria for Inclisiran – Consider treatment | Likely to be eligible for inclisiran treatment | Consider treatment |
Lipid Management – Primary Prevention
| Report Name | Report Returns | Notes |
| ? Lipids 6.1 Primary Prevention – Possible poor lipid lowering therapy concordance | Patients with repeat lipid lowering who have not been issued a prescription in the last 3 months. | Review patient – discuss concordance or remove medication from repeat if no longer necessary. |
| ? Lipids 6.2 Primary Prevention – Consider starting lipid lowering | Patients who appear eligible for lipid lowering for primary and secondary prevention who don’t have recorded reason why not. | Review patient: consider offering statin or other treatment recording ‘declined, not indicated’ etc. Record previous ADRs to lipid lowering treatment. |
| ? Lipids 6.3 Primary Prevention – Consider setting lipid target | Patients with repeat lipid lowering therapy who do not have a lipid target. | Review patient – consider adding target. The Lipid Details Template will facilitate this. |
| ? Lipids 6.4 Primary Prevention – Lipid target set but not achieved | Patients with a lipid target which has not been achieved | Consider intensification of lipid treatment or relaxation of target (e.g. for frail patients). |
| ? Lipids 6.5 Primary Prevention – On low/mod LLT – Consider LLT intensification | Patients on low or moderate potency lipid lowering without a documented reason. | Review patient. Consider: Intensification coding of previous ADRs to lipid lowering recording patient has reached maximally tolerated lipid lowering. Loosen target cholesterol. |
| ? Lipids 6.51 Primary Prevention – On low/mod LLT – Consider LLT intensification (unless target already achieved) | As for 6.5 but excludes patients who have reached their target cholesterol | As Above. |
Lipid Management – Secondary Prevention
| Report Name | Report Returns | Notes |
| ? Lipids 7.1 Secondary Prevention – Possible poor lipid lowering therapy concordance | Patients with repeat lipid lowering who have not been issued a prescription in the last 3 months. | Review patient – discuss concordance or remove medication from repeat if no longer necessary. |
| ? Lipids 7.2 Secondary Prevention – Consider starting lipid lowering | Patients who appear eligible for lipid lowering for primary and secondary prevention who don’t have recorded reason why not. | Review patient: consider offering statin or other treatment recording ‘declined, not indicated’ etc. Record previous ADRs to lipid lowering treatment. |
| ? Lipids 7.3 Secondary Prevention – Consider setting lipid target | Patients with repeat lipid lowering therapy who do not have a lipid target. | Review patient – consider adding target. The Lipid Details Template will facilitate this. |
| ? Lipids 7.4 Secondary Prevention – Lipid target set but not achieved | Patients with a lipid target which has not been achieved | Consider intensification of lipid treatment or relaxation of target (e.g. for frail patients). |
| ? Lipids 7.5 Secondary Prevention – On low/mod LLT – Consider LLT intensification | Patients on low or moderate potency lipid lowering without a documented reason. | Review patient. Consider: Intensification coding of previous ADRs to lipid lowering recording patient has reached maximally tolerated lipid lowering. Loosen target cholesterol. |
| ? Lipids 7.51 Secondary Prevention – On low/mod LLT – Consider LLT intensification (unless target already achieved) | As for 6.5 but excludes patients who have reached their target cholesterol | As Above. |
| ? Lipids 7.6 Secondary Prevention – Consider intensification to very high intensity lipid lowering | Patients eligible for secondary prevention who are not on very high intensity lipid lowering. | Review patient. Consider Intensification coding of previous ADRs to lipid lowering recording patient has reached maximally tolerated lipid lowering. Loosen target cholesterol. |
| ? Lipids 7.61 Secondary Prevention – Consider intensification to very high intensity lipid lowering (unless target already achieved) | As for 4.4 but excluding patients who have reached their target cholesterol. | As Above. |
| ? Lipids 7.7 Secondary Prevention – Consider intensification – ASCVD and LDLC >2.6 | Patients with established atherosclerotic ASCVD with nonHDL C unless they have achieved a stated target. | Review patient. Consider Intensification coding of previous ADRs to lipid lowering recording patient has reached maximally tolerated lipid lowering. Loosen target cholesterol. |
| ? Lipids 7.71 Secondary Prevention – Consider intensification – ASCVD and LDLC >2.6 (unless target nonHDL already achieved) | As for 7.7 but excluding patients who have a lipid target and have achieved this target. | As above. |
| ? Lipids 7.72 Secondary Prevention – Consider intensification – ASCVD and LDLC >2.6 (target nonHDL set and already achieved) | As for 7.7 but including patients who have a lipid target and have achieved this target. |
Performance Reports
The following reports in the CDRC Performance > Lipids folder will provide a picture of your practice’s lipid management performance.
Overview
| Report Name | Report Returns |
| 1 Lipids – Overview 1.0 – Proportion of population on Lipid Rx | Number of people with lipid lowering therapy on repeat prescription |
| 1 Lipids – Overview 1.1 On Lipid Rx with issue in last 3m | Number of people with lipid lowering therapy on repeat prescription who have had a prescription in the last 3 months |
| 1 Lipids – Overview 1.2 On Lipid Rx with lipid target | Number of people with lipid lowering therapy on repeat prescription who have a recorded lipid target |
| 1 Lipids – Overview 1.21 On Lipid Rx with lipid target and target achieved | Number of people with lipid lowering therapy on repeat prescription who have achieved their lipid target |
| 1 Lipids – Overview 2.0 Has indication for lipid lowering | All patients who appear to have a good indication for lipid lowering (primary and secondary prevention) |
| 1 Lipids – Overview 2.1 Has indication for lipid lowering on lipid lowering | The number of patients in 2.0 who have lipid lowering medication on repeat |
| 1 Lipids – Overview 2.11 Has indication for lipid lowering on lipid lowering (high/very high intensity) | The number of patients in 2.0 who have high/very high intensity lipid lowering medication on repeat |
| 1 Lipids – Overview 2.2 – Proportion where Lipid Rx indicated but not treated nor reason recorded | Number of people who appear eligible for lipid lowering who do not have: Lipid lowering on repeat A clear reason for not using lipid lowering |
| 1 Lipids – Overview 3.0 – Proportion of patients to target for CVD risk assessment | Number of patients with an estimated CVD risk >=10% who should be offered a formal CVD risk assessment |
Secondary Prevention
| Report Name | Report Returns |
| 2 Lipids – ASCVD 1.0 Has manifest atherosclerosis (ASCVD) | Patients with AAA, CHD, PAD, ischaemic/unclassified stroke or TIA |
| 2 Lipids – ASCVD 1.1 Very high intensity lipid lowering | Established ASCVD and on very high intensity lipid lowering |
| 2 Lipids – ASCVD 1.2 On high/very high intensity lipid lowering | Established ASCVD and on high or very high intensity lipid lowering |
| 2 Lipids – ASCVD 1.3 On high/very high intensity Rx OR On low/mod intensity Rx with reason # | Established ASCVD: on high or very high intensity lipid lowering OR On low or moderate intensity lipid lowering with maximal tolerated lipid lowering recorded in the last year OR Atorvastatin ADR recorded |
| 2 Lipids – ASCVD 1.4 On lipid lowering | Established ASCVD on any lipid lowering |
| 2 Lipids – ASCVD 1.41 On lipid lowering – issued in the last 3 months | Established ASCVD on any lipid lowering AND issued in the last 3 months |
| 2 Lipids – ASCVD 1.42 On lipid lowering – with cholesterol target | Established ASCVD on lipid lowering therapy with a record of a lipid target (usually non-HDL cholesterol) |
| 2 Lipids – ASCVD 1.421 On lipid lowering – with cholesterol target – target achieved | As 1.42 with target achieved |
| 2 Lipids – ASCVD 1.5 On lipid lowering OR Reason why not | Established ASCVD on any lipid lowering or clear reason why not – should be aiming for 100% |
Familial Hypercholesterolemia
| Report Name | Report Returns |
| 3 Lipids – FH 1.0 Definite or probable | Definite or probable familial hypercholesterolaemia |
| FH reports 1.1 – 1.5 as for the ASCVD reports above |
Primary Prevention
| Report Name | Report Returns |
| 4 – Lipids – PP 1.0 Primary Prevention Indicated | Primary prevention by lipid modification is likely to be recommended for these patients |
| PP report 1.1 – 1.6 as for the ASCVD report above |
CVD Risk Assessment
| Report Name | Report Returns |
| 5 Lipids – Assess CVD Risk 1 – estimated risk >=10% | Patients whose estimated 10 year risk of CVD is >=10% who have not had a formal risk assessment. |
| 5 Lipids – Assess CVD Risk 2 – Already on lipid lowering without risk assessment | Patients on lipid lowering without an obvious indication. |
Statin Safety Reports
The following reports will identify important statin safety issues. Use the Lipid Lowering template to help.
The following reports are found in the CDRC Quality > Lipids folder:
| Report Name | Report Returns | Notes |
| ? Statin Safety 1.0 – Any statin – potential contraindicated interaction # | Patients on repeat statin and another medication that appears to be contraindicated | Review patient medication to ensure safety |
| ? Statin Safety 1.1 – Simvastatin – ! MHRA ! Any potential contraindicated interaction # | (Subset of 1.0 above) Patients on simvastatin with a contraindicated medication in line with the MHRA warning | Review record https://www.gov.uk/drug-safety-update/simvastatin-updated-advice-on-drug-interactions |
| ? Statin Safety 2.0 – Any statin – caution, potential interaction # | Patients on repeat statin and another medication where caution is recommended | Review patient medication to ensure safety |
| ? Statin Safety 3.0 – Any statin – consider dose in view of eGFR # | Patients on repeat statin whose renal function indicates that dose alteration MAY be needed | Review patient medication to ensure safety |
Recommended Batch Reporting
Consider running the follow reports in automatic batches so the relevant professional or group are notified about patients to review at appropriate interval. For more details on setting this up see Automated Reporting
Monthly Batch
| Report Name | Report Location | Report Return | Notes |
| ? Lipids 3.2 Management – Possible poor lipid lowering therapy concordance # | CDRC Quality > Lipids | Patients who don’t seem to be taking their prescribed lipid lowering | Contact patient to review concordance |
| Lipids > ? Statin Safety 1.0 – Any statin – potential contraindicated interaction # | CDRC Quality > Lipids | Patients with potential serious statin interactions. | Use Lipid Lowering Template to review potential serious interactions |
Quarterly Batch
| Report Name | Report Location | Report Returns | Notes |
| ? Statin Safety 3.0 – Any statin – consider dose in view of eGFR | CDRC Quality > Lipids | Patients who may need dose adjustments based on renal function | Review record. Consider suitability of statin dose given eGFR |
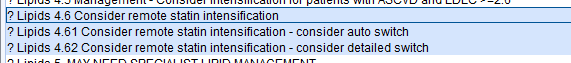
| ? Lipids 4.6 Consider remote statin intensification | CDRC Quality > Lipids | Patients who could have an electronic invite to consider statin intensification | |
| ? Lipids 1.04 Screening – Target for CVD Risk Assessment – estimated risk >20% | CDRC Quality > Lipids | Patients at highest risk of CVD who have not had a CVD risk assessment | Consider inviting for a CVD risk assessment. |
Annual Batch
| Report Name | Report Location | Report Returns | Notes |
| ? Lipids 2.0 Case Finding – Consider screening for familial hypercholesterolaemia # | CDRC Quality > Lipids | Patients who may have familial hypercholesterolaemia | Review record and refer if appropriate |
| ? Lipids 4.3 Management – On low/mod lipid lowering – consider intensification # | CDRC Quality > Lipids | Patients to consider for lipid lowering intensification | Review patient and consider intensification or recording maximally tolerated treatment |
| ? Lipids 4.4 Management – Consider intensification to very high intensity lipid lowering # | CDRC Quality > Lipids | Patients to consider for lipid lowering intensification (secondary prevention only) | Review patient and consider intensification or recording maximally tolerated treatment |
| ? Lipids 5.1 Management – Consider lipid lowering – May need more detailed input | CDRC Quality > Lipids | Patients with more complex lipid issues e.g. previous intolerance to statin AND ezetimibe | Review record and consider treatment/referral |
| ? Lipids 5.4 Management – Referral Criteria for PCSK9i – Consider referral | CDRC Quality > Lipids | Patients who might benefit from PCSK9i treatment | Consider offering a referral to local lipid clinic |
| Diabetes DM022 | Potential Fix – Consider adding SNOMED code for statin ADR | CDRC Contracting > QoF | Diabetic patients who are missing from the diabetes over 40 statin QoF indicator – with a record of an S1 adverse reaction to statin but no SNOMED code | Consider adding SNOMED code – no clinical benefit but helps with performance measures. |
| Diabetes DM023 | Potential Fix – Consider adding SNOMED code for statin ADR | CDRC Contracting > QoF | Diabetic patients who are missing from the diabetes and CVD statin QoF indicator – with a record of an S1 adverse reaction to statin but no SNOMED code | Consider adding SNOMED code – no clinical benefit but helps with performance measures. |
Batch Contacting Patients to Consider Lipid Lowering Intensification
The following process allows quick and effective contact with patients to consider intensification of lipid lowering therapy.
- Use these reports to identify people who might eligible for the process. Criteria are:
- Not manifest atherosclerosis
- Not previous tried high intensity statin
- Not clear reason to avoid high intensity statin
- Not declined intensification in the last year
- Use the communications annexe to send selected patients the following message and questionnaire. Add the code Offer of statin therapy to invited patients. Patients without a mobile number or email address will need to be contacted in a different way e.g. phone or letter.
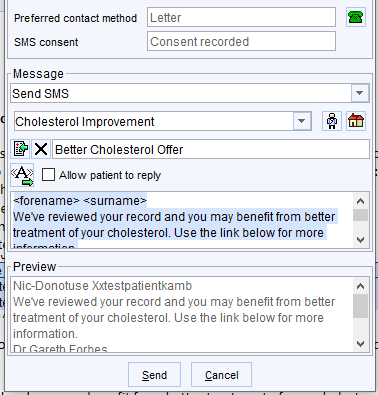
This is the text to cut and paste into the message – a preset can be created for future use.
<forename> <surname>
We’ve reviewed your record and you may benefit from better treatment of your cholesterol. Use the link below for more information.
<staff_member_title> <staff_member_forename> <staff_member_surname>
- The patient will receive the following questionnaire. Replies will appear as a task in SystmOne
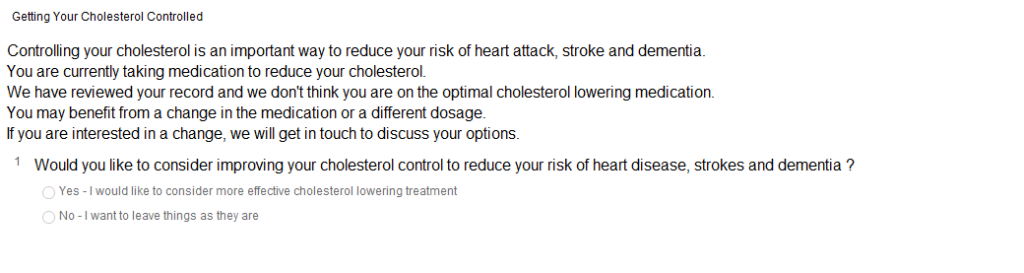
Patients who answer ‘yes’ can be contacted. To discuss intensification. The two sub-reports 4.61 and 4.62 divide patients into those who are likely to be relatively simple (only been on one statin previously) or more complicated (multiple previous statins or previous high intensity statins).
Patients who answer ‘no’ should have the code Patient on maximal tolerated lipid lowering therapy added.
