The CDRC has developed a suite of Population Reporting Searches to support you with the detection, intervention and management of patients with diagnosed and undiagnosed cardiovascular diseases including, Atrial Fibrillation (AF), Coronary Heart Disease (CHD) and Hypertension.
Concordance Alerts and Drugs to Diagnosis Population Reporting Searches are also included within the .zip file below.
Accessing the Cardiovascular Population Reporting Searches
To access the CDRC Cardiovascular Population Reporting Searches on EMIS, you will need to download and import the following .zip file:
If you have not performed this process before, please refer to the Download/ Import guide below, which provides you with step-by-step instructions on how to Download and Import .zip files into EMIS:
Please note: do not use the CDRC Cardiovascular Subreports folder contained within this.zip file, searches within this folder are used to build the primary searches noted in the guidance below.
You can check whether you have the most up-to-date version by reviewing the date on the .zip file. Any updates to the Population Reporting searches will be communicated to CDRC Precision users via the mailing list for the CDRC. To ensure you stay up to date with the latest information, please sign up to the mailing list at http://eepurl.com/9131L
Guidance on the Atrial Fibrillation (AF) Population Reporting Searches
The primary Population Reporting Searches for AF are highlighted below along with the patient’s returned from these searches.
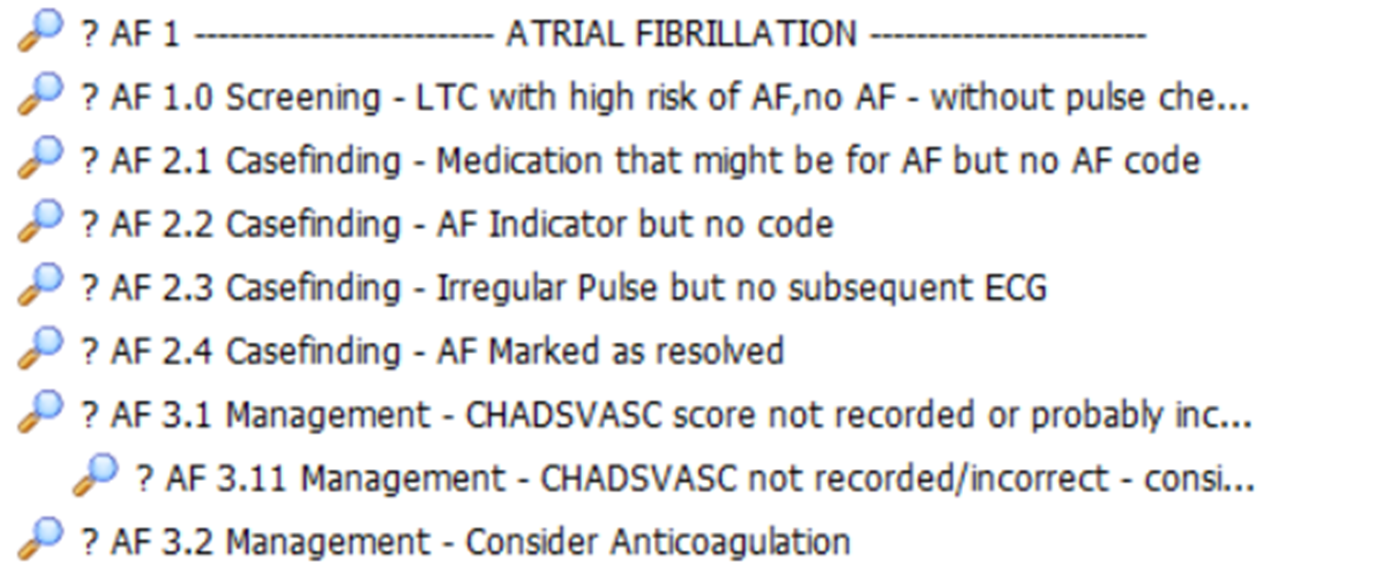
| Search Name | Patient’s Returned |
| ? AF 1.0 Screening – LTC with high risk of AF, no AF – without pulse check 12m | Patients not diagnosed with AF but have a long term condition that has a high risk of AF and no pulse check performed in the last 12 months. |
| ? AF 2.1 Casefinding – Medication that might be for AF but no AF code | Patients on rate limiting calcium channel blockers, beta-blockers, digoxin or amiodarone without obvious coded indication for these drugs. Also likely to detect patients with other uncoded diagnoses such as hypertension and heart failure. |
| ? AF 2.2 Casefinding – AF Indicator but no Read Code | Patients with codes suggestive of AF but no QoF code e.g. H/O Atrial fibrillation |
| ? AF 2.3 Casefinding – Irregular Pulse but no subsequent ECG | Patients who have an irregular pulse without a subsequent ECG. Some of these patients will have erroneous entries of irregular pulse. |
| ? AF 2.4 Casefinding – AF Marked as resolved | Patients who have previously had AF which is currently marked as resolved AF resolved should not be used for patients with paroxysmal AF who are not currently in AF. |
| ? AF 3.1 Management – CHADVASC score not recorded or probably incorrect | Patient with AF who do not have a CHADSVASc score or whose most recently recorded score may be incorrect. Review patient and add/update score if appropriate. |
| ? AF 3.11 Management – CHADVASC score not recorded/incorrect – consider anticoag | As above, consider the patient for Anticoagulants. |
| ? AF 3.2 Management – Consider Anticoagulation | Patients with AF and moderate or high stroke risk who are not anticoagulated and do have an expiring exception in the last year or a persistent exception. Review the patient and consider anticoagulation or record exception if appropriate. |
Guidance on the Coronary Heart Disease (CHD) Population Reporting Searches
The primary Population Reporting Searches for CHD are highlighted below along with the patient’s returned from these searches.
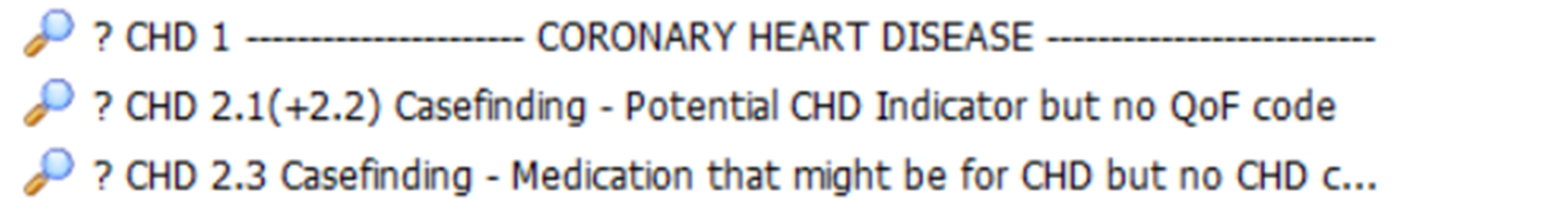
| Search Name | Patient’s Returned |
| ? CHD 2.1 (+2.2) Casefinding – Potential CHD Indicator but no QoF code | Patients with codes suggestive of CHD but no QoF code. |
| ? CHD 2.3 Casefinding – Medication that might be for CHD but not CHD code | Patients on antianginals, nitrates, RAS, prasugrel or ticagrelor, calcium channel blockers, beta-blockers without obvious coded indication for these drugs. Patient not coded with CHD. |
Guidance on the Heart Failure Population Reporting Searches
The primary Population Reporting Searches for Heart Failure are highlighted below along with the patient’s returned from these searches.
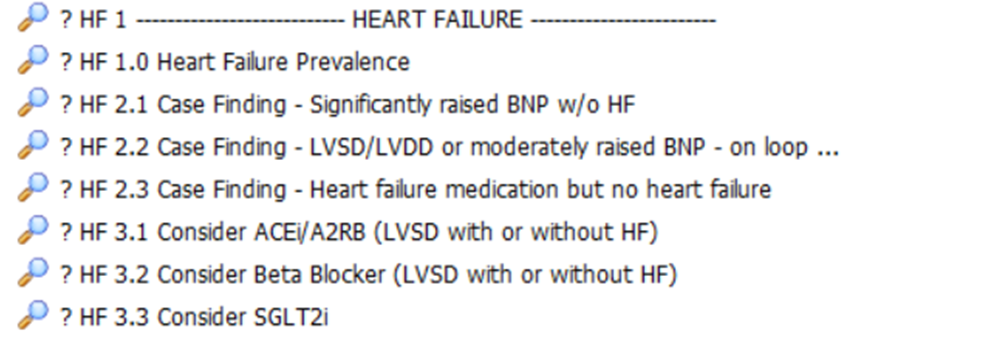
| Search Name | Returns | Notes |
| ? HF 1.0 Heart Failure Prevalence | All patients with Heart Failure | |
| ? HF 2.1 – Case Finding – Significantly raised BNP w/o HF | Patients with a significantly raised BNP without diagnosis of heart failure. | Review record. |
| ? HF 2.2 – Case Finding – LVSD/LVDD or moderately raised BNP – on loop diuretic | Patients taking loop diuretics with LV systolic or diastolic dysfunction or a raised BNP. | Review record. |
| ? HF 2.3 – Case Finding – Heart failure medication but no heart failure diagnosis | Patients taking spironolactone/eplerenone/sacubitril without obvious reason. (will detect some patients being given spironolactone for resistant hypertension) | Review record. |
| ? HF 3.1 Consider ACEI/A2RB (LVSD with or without HF) | Patients with Heart Failure with reduced ejection fraction or LVSD not currently on a repeat ACEi/A2RB. | Review record and consider for ACEi/A2RB. |
| ? HF 3.2 Consider Beta Blocker (LVSD with or without HF) | Patients with Heart Failure with reduced ejection fraction or LVSD not currently on a repeat Beta Blocker. | Review record and consider for Beta Blocker. |
| ? HF 3.3 Consider SGL2Ti | Patients with Heart Failure on a repeat ACEi/A2RB and a Beta Blocker. | Review record and consider for SGLT2i. |
Guidance on the Hypertension Population Reporting Searches
The primary Population Reporting Searches for Hypertension are highlighted below along with the patient’s returned from these searches.
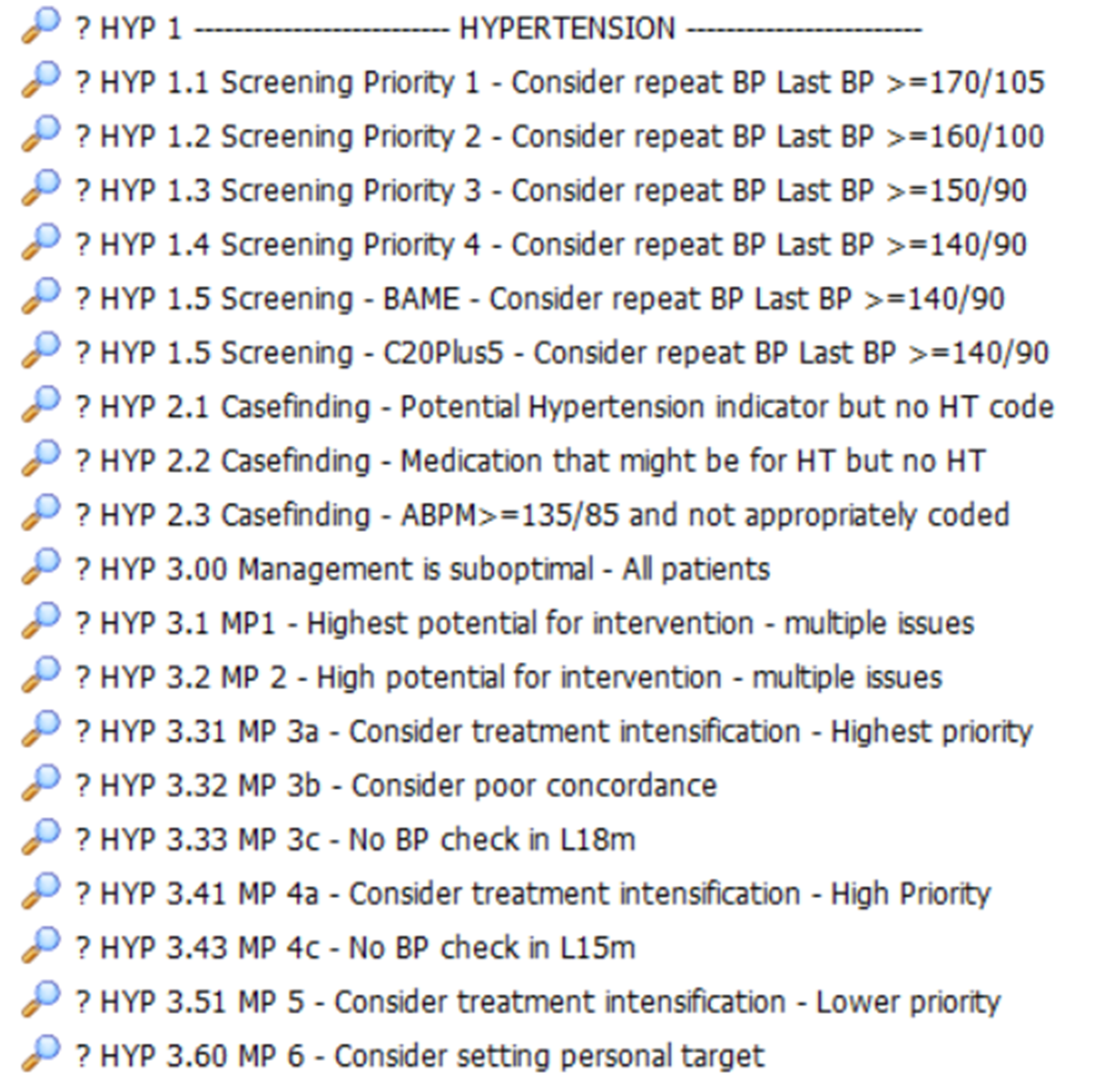
| Search Name | Patient’s Returned |
| ? HYP 1.1 Screening Priority 1 – Consider repeat BP Last BP >=170/105 | Patient’s not coded with hypertension whose last blood pressure was >=170/105. Consider inviting patient for a BP reading. |
| ? HYP 1.2 Screening Priority 2 – Consider repeat BP Last BP >=160/100 | Patient’s not coded with hypertension whose last blood pressure was >=160/100. Consider inviting patient for a BP reading. |
| ? HYP 1.3 Screening Priority 3 – Consider repeat BP Last BP >=150/90 | Patient’s not coded with hypertension whose last blood pressure was >=150/90. Consider inviting patient for a BP reading. |
| ? HYP 1.4 Screening Priority 4 – Consider repeat BP Last BP >=140/90 | Patient’s not coded with hypertension whose last blood pressure was >=140/90. Consider inviting patient for a BP reading. |
| ? HYP 1.5 Screening – BAME – Consider repeat BP Last BP >=140/90 | BAME patient’s not coded with hypertension whose last blood pressure was >=140/90. Consider inviting patient for a BP reading. |
| ? HYP 1.5 Screening – C20Plus5 – Consider repeat BP Last BP >=140/90 | Core20Plus5 patient’s not coded with hypertension whose last blood pressure was >=140/90. Consider inviting patient for a BP reading. |
| ? HYP 2.1 Casefinding – Potential Hypertension Indicator but no HT code | Patients with a code to suggest hypertension (e.g. hypertension annual review) without a QoF hypertension code. |
| ? HYP 2.2 Casefinding – Medication that might be for HT but no HT | Patients on medication which might be for hypertension without a hypertension code |
| ? HYP 2.3 Casefinding – ABPM >=135/85 and not appropriately coded | Home BP average reading >=135/85 (defines hypertension) without a subsequent hypertension code. |
| ? HYP 3.00 Management is suboptimal – All patients | |
| ? HYP 3.1 MP1 – Highest Potential for intervention – multiple issues | Priority 1 Has all three: – 3 months overdue BP check – Suspected poor concordance – BP is >20/10 over NICE or personal target |
| ? HYP 3.2 MP 2 – High Potential for intervention – multiple issues | Priority 2 Have two out of three: – 3 months overdue BP check – Suspected poor concordance – BP is >20/10 over NICE or personal target |
| ? HYP 3.31 MP 3a – Consider treatment intensification – Highest priority | Priority 3a Last BP >30/15 above NICE or personal target. Priority 1 and 2 patients excluded. |
| ? HYP 3.32 MP 3b – Consider poor concordance | Priority 3b Need BP control who do not appear to be collecting antihypertensive. Priority 1 and 2 patients excluded. |
| ? HYP 3.33 MP 3c – No BP check in L18M | Priority 3c Need BP check, >=6 months overdue. Priority 1 and 2 patients excluded. |
| ? HYP 3.41 MP 4a – Consider treatment intensification – Higher priority | Priority 4a Last BP >20/10 above NICE or personal target. Priority 1 and 2 patients excluded. |
| ? HYP 3.42 MP 4c – No BP check in L15M | Priority 4c Need BP check, >=3- months overdue. Priority 1 and 2 patients excluded. |
| ? HYP 3.51 MP 5 – Consider treatment intensification – Lower priority | Priority 5 Last BP above NICE or personal target. Priority 1 and 2 patients excluded. |
| ? HYP 3.6 MP 6 – Consider setting personal target | Priority 6 Need BP control but do not have a personal target. Consider setting personal target. |
