CDRC can be configured to deliver Long Term Condition (LTC) Call and Recall.
Each unit defines the LTCs that they wish to include in their call/recall system. Any condition that can be systematically recorded can be included. Most practices will include the QoF LTCs. Common additional conditions include:
- Patients at high risk of diabetes – NDH/IGR/history of gestational diabetes/PCOS
- Non-QoF respiratory diseases – E.g. pulmonary fibrosis, bronchiectasis
- Non-alcoholic fatty liver disease
- Coeliac disease
- Familial hypercholesterolaemia
- Gout
- Frailty
Additionally, customised lists of patients with specific needs can also be created, e.g. patients on watchful waiting prostate cancer management.
LTC Recall
Each patient with a relevant LTC is given a single ‘LTC Recall’ recall date. This replaces all previous condition specific recalls e.g. asthma recall, diabetes recall. The default is to set the recall in the month of birth but it can be set to any time of the year.
Quality Control
Automatic Quality Control searches are set to monitor the system to identify patients who need a LTC recall who do not have a pending recall e.g. new patients, patients with a new diagnosis, patients where the LTC recall date has been accidentally set too far in the future or in the past. A task is sent to the administration team at regular intervals, defined by the practice, to identify these patients.
Running The Searches
The LTC admin team defines the week they want to run the recall system. Lists of relevant patients are then created.
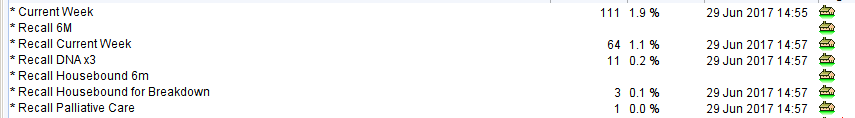
The above screenshot shows a typical set of reports but this can be customised for each unit.
Recall Current Week – will display all those patients who are due a LTC recall this week, or 4 weeks ago or 8 weeks ago. This allows the patients to be invited at monthly intervals as required by QoF. Patients who are housebound or on the palliative care list are excluded.
Recall 6M – identifies patients who need a 6 month review. The default setting is that 6m recalls will be generated for:
- Patients with Diabetes (unless they are in remission)
- Patients with CKD severe enough to warrant 6 month assessment (as defined by NICE)
Recall Housebound and Housebound 6M – similar to the above reports but for housebound patients who are likely to need a different management pathway.
Recall DNAx3 – patients who have not attended LTC review after three invitations. The unit can then decide how to manage these patients e.g. exception report, further attempts to contact.
Recall Palliative Care – a list of patients with LTCs but also on the palliative care list. The recommended approach is to arrange clinician review of the patient’s record and make an individual decision about whether a ‘standard’ LTC review is needed (e.g. stable palliative patients) or whether alternative provision is needed.
Invitation
The unit can use the lists created above to arrange invitations. Invitations can be sent by post, SMS text message or email. The unit can choose to send appointments or invitations to make an appointment.
Conducting a Review
When the patient is seen for review the clinician uses the LTC Master template. This displays the conditions the patient has, previous reviews and the most recent LTC recall information. The tests the patient needs are displayed along with other ‘tasks’ such as need for immunisation, screening (NHS Health Checks, diabetes screening etc.) and drug monitoring tests.
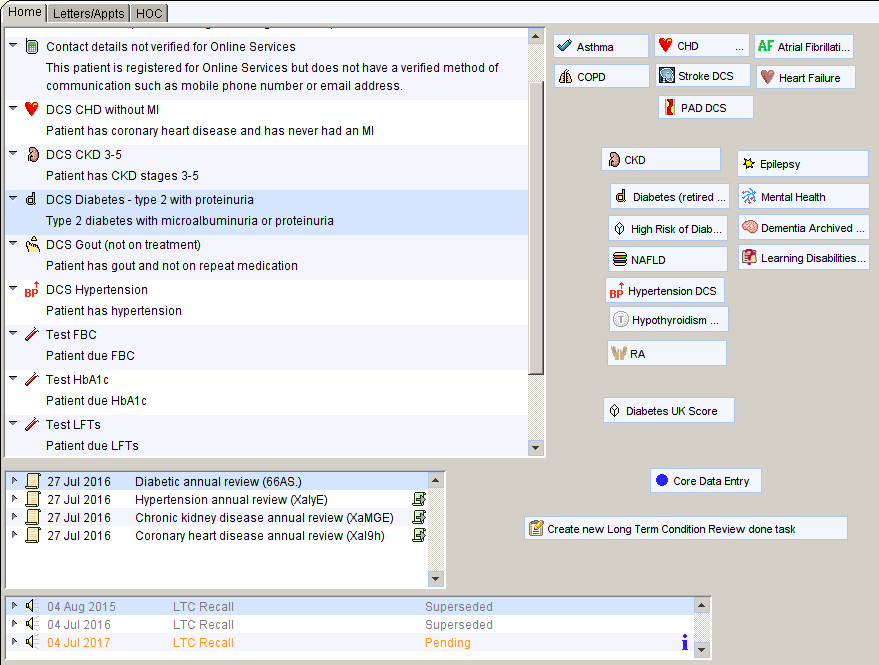
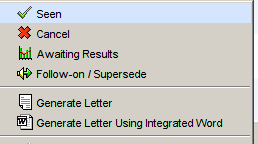
The clinician then completes the basic information needed for almost all reviews e.g. weight, smoking, lifestyle via the Core Data Entry button, then works their way through the conditions that the patient has completing the information/interventions specific to that condition. For some combination of conditions and depending on the skill mix at the unit, this might be done over more than one appointment. Once all the conditions have been reviewed, the LTC Recall date is reset by right clicking on the most recent LTC recall. The user will be prompted to entering a new LTC recall date in 1 year. The user does not need to set any routine 6 month reviews – these are automatically created based on the annual LTC review.
If an interim review is deemed necessary that wouldn’t be part of routine care (e.g. a patient with diabetes needs a review at 3 months) the scheduled task function is used to generate this follow up.
Advanced Options
If needed a unit can set up a more advanced recall system based on the skill mix in their unit. This aims to maximise the efficient use of staff whilst minimising inconvenience for patients.
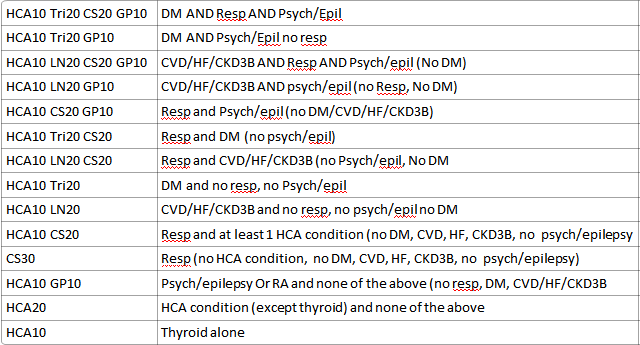
The unit defines the pathways that patients will follow depending on staff competencies.
A simple example:
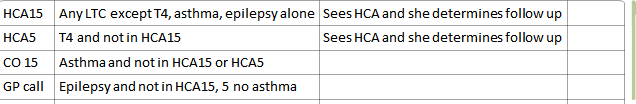
A complex example:
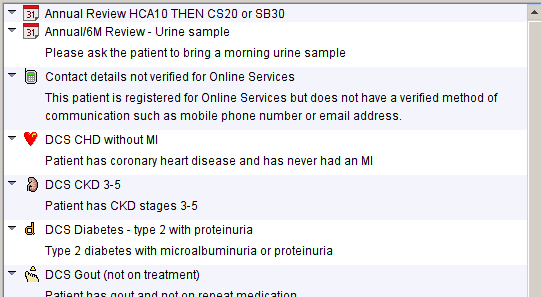
Patients are sent an invitation asking them to contact the surgery to arrange their appointment. When the patient rings, admin/reception staff can easily see what pathway the patient requires. In the example below, the patient needs a 10 minute appointment with the HCA for blood tests and then an appointment with one of the practice nurses (different times due to different levels of experience). It also prompts the admin staff to remind the patient to bring a urine sample if needed.
Advantages of the System
- Extremely simple for the user.
- Can be very complex
- Allows any number of LTC conditions to be managed in one system
- Integrated care
- Quality control built in to ensure no patients are missed
- Significantly reduces to possibility of problems due to user error e.g. forgetting to add recall dates or setting the wrong recall
- Evidence based
- Can maximise use of staff
- Minimises inconvenience and duplication for patients
Appendices
Appendix 1 – Disease Specific Recalls
Disease specific recalls that are counted in the recall recovery system:
- Asthma
- Asthma annual review
- Atrial fibrillation
- Atrial Fibrillation Annual Review
- CHD
- CHD Annual Review
- CHD Monitoring
- CHRONIC DISEASE MANAGEMENT
- Chronic Disease Monitoring
- Chronic Disease Review
- Chronic Disease Review 12m
- Chronic Disease Review 3m
- Chronic Disease Review 6m
- CKD
- COPD
- COPD ANNUAL REVIEW
- Coronary Heart Disease annual review
- DEMENTIA
- Dementia Annual Review
- Dementia Review
- Diabetes
- Diabetes 3month Review
- Diabetes 6 month check
- Diabetes 6 month review
- Diabetes 6month review
- Diabetes Annual Review
- DIABETES MELLITUS
- Diabetic 6 month review
- Diabetic Annual Review
- Epilepsy
- Heart Failure
- Heart Failure Annual Review
- Hypertension
- HYPERTENSION ANNUAL REVIEW
- Hypertension Monitoring
- Hypothyroidism
- hypothyroidism annual review
- Learning Disabilities
- PVD Monitoring
- Rheumatoid Annual Review
- Rheumatoid Arthritis
- Rheumatoid Arthritis Annual Review
- Rheumatoid Arthritis Monitoring
- Stroke
Appendix 2 – Higher Risk Patients
| Higher Risk | |
| Any LTC | >=4 DNAs in the past 2 years Significantly overdue drug monitoring |
| Asthma | >6 SABA in last 12 months Last ACT score >20 LABA on repeat and no ICS High dose ICS LAMA Aminophylline Biologics Likely moderately severe asthma Exacerbations (>2 in 12, severe/admission last 12m, life threatening) Exacerbation in last 2y but no ICS Concordance issue – LABA, LAMA Exceeding usual quantities of long acting inhalers |
| AF | Anticoagulation should be considered |
| CHD | BP > 150/90 Poor concordance (anticoagulants, antiplatelets, betablocker, ccb, diuretics, RAS drugs, statin) |
| CKD | CKD G3aA3, G3bA2,3, G4/5 |
| COPD | Severe COPD MRC 4+5 >=3 exacerbations in the last year >=3 course of prednisolone in the last year CAT score >20 Concordance issues with long term inhalers |
| Diabetes | Scoring system (1 point for each of) Hba1c>100 Hba1c >75 Hba1c >58 BP >=150/90 High risk feet Mod risk feet ACR >3 ACR>30 Lipid Total Cholesterol>5 Poor concordance hypoglycaemics Poor concordance lipid lowering Poor concordance RAS drugs Poor concordance diuretics Poor concordance CCBs Score >=3 |
| Heart failure | NYHA 3 and 4 Sicubatril Eplerenone, spironolactone |
| Hypertension | BP>=150/90 Poor concordance beta blockers Poor concordance alpha blockers Poor concordance lipid lowering Poor concordance RAS drugs Poor concordance diuretics Poor concordance CCBs |
| Learning disability | BMI <19 or >40 On antidepressants, antipsychotics, anxiolytics, hypnotics, opioids, gabapentinoids, lithium Two or more (non LD) LTCs No health check for 2 years History of aspiration pneumonia or PEG Any drug monitoring is significantly overdue |
| PAD | BP > 150/90 Poor concordance (anticoagulants, antiplatelets, betablocker, ccb, diuretics, RAS drugs, statin) |
| Stroke | BP > 150/90 Poor concordance (anticoagulants, antiplatelets, betablocker, ccb, diuretics, RAS drugs, statin) |
