Patients who may have Familial Hypercholesterolmaemia (FH) can be identified in the following reports in the folder CDRC Quality > Lipids
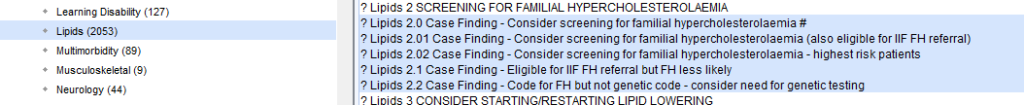
| Report Name | Report Returns | Action |
| ? 2.0 Case Finding – Consider screening for familial hypercholesterolamia | Patients who have a significant chance of familial hypercholesterolaemia | Screen for FH – see below |
| ? 2.01 Case Finding – Consider screening for familial hypercholesterolamia (also eligible for IFF FH referral) | Patients in 2.0 who are also appear in the IIF CVD04 ‘consider for FH assessment’ denominator | Screen for FH – see below |
| ? 2.02 Case Finding – Consider screening for familial hypercholesterolamia – highest risk patients | Patients in 2.0 who are at highest risk of FH – for areas with limited resources – concentrate on these patients | Screen for FH – see below |
| ? 2.1 Case Finding – Eligible for IFF FH referral but FH less likely | Patients who appear in the IIF CVD04 ‘consider for FH assessment’ denominator, who are less likely to have FH | Screen for FH – see below, but likely to have a secondary cause of hyperlipidaemia |
| ? 2.2 Case Finding – Code for FH but not genetic code – consider need for genetic testing | Patients with a code suggesting FH e.g. Possible FH who don’t have a definitive FH code | Review record and consider: Adding definitive code if appropriate Referral for genetic testing Removal of code if incorrect – e.g. secondary hyperlipidaemia |
Patients are identified using a combination of tools – NICE guidance, estimated Dutch Lipid Clinic Network scores and estimated Welsh FH Score with adjustment for high triglyceride levels.
Two pages of the Lipids Details Template will help with screening
- Aetiology page – page showing information about possible causes of hyperlipidaemia, especially, secondary causes – Aetiology of Abnormal Lipids
- FH Screening page – calculate the Dutch Lipid Clinic Network Score. Local referrals protocols vary, but patients with a DLCNS >=6 are usually referred to a lipid clinic to consider FH genetic testing.
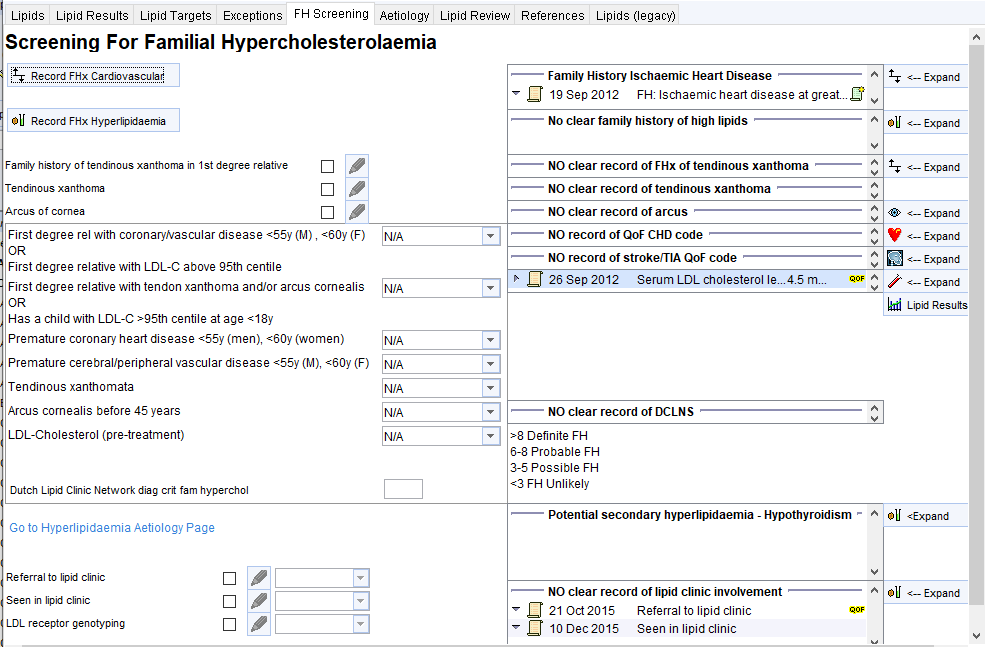
The central panel shows relevant information from the record and the buttons on the left allow this information to be expanded.
Record the following if not already recorded:
- Family history of CVD and/or hyperlipidaemia
- Family history of tendinous xanthomata
- History of tendinous xanthomata
- History of arcus
Then use this information to calculate a Dutch Lipid Clinic Network Score.
Consider secondary causes of hyperlipidaemia such as uncontrolled diabetes mellitus, untreated hypothyroidism, chronic renal failure, nephrotic syndrome, cholestasis, hypopituitarism, anorexia, obesity, anticonvulsants, antipsychotics, steroids, cyclosporin, anti-retrovirals, retinoids. Some of these issues will be shown in the panel towards the bottom of the template.
Use the bottom boxes to record referral to or consultation in lipid clinics (recent or historic)
Calculating the highest LDL-cholesterol
It can be difficult to find a pre-treatment LDL-cholesterol in some patients who have been on lipid lowering therapy for many years. The Lipids Results button will show all previous lipid results to help with this.
The LDL-C can be estimated using Friedewald equation:
- LDL-C = non-HDL-C minus (triglycerides / 2.2).
- This formula is not valid if the triglyceride level is >=4.5. In addition the DLCNS is not valid if the lipid values are associated with a triglyceride level >2.3.
In the example below the pre-treatment non-HDL can be estimated by subtracting the HDL (estimated at around 1, looking at subsequent values) from the total cholesterol, e.g. 8.2-1 = 7.2
Then estimating that the pre-treatment triglyceride level was around 3, LDLC= 7.2-3/2.2 = ~5.8
![Graph
Data Settings Graph
Preset All Lipid Tests (BC)
Z] Only show readings that the patient has at least one of
Edt Presets
Date
25 dui 2003
30 Dec 2003
01 Mar 2004
01 Mar 2004
01 Mar 2004
20 May 2004
02 Aug 2004
08 Nov 2004
08 Nov 2004
07 Mar 2005
06 Dec 2005
28 Feb 2006
04 Dec 2006
21 Mar 2007
02 Nov 2007
08 Dec 2008
16 Nov 200g
20 Jan 2010
lgMay 2010
IODec 2010
21 Dec 2011
13 Dec 2012
dan 2014
14 Jan 2015
11 Dec 2015
02 Dec 2016
30 Nov 2017
Serum LDL choL„ Serum choleste
Serum HDL chu
06
1 43
Serum choleste
Serum triglyceride levels
401
1 32
221
236](https://cdrc.nhs.uk/wp-content/uploads/2022/11/image-28.png)
This patient’s lipid profile is highly suggestive of metabolic syndrome rather than FH, with low HDL-C, raised TGs and a BMI of >35.
